-10:11am Tuesday, June 5, 2006: This was the moment Marge was told the mammogram showed a mass, which was probably breast cancer. “But, don’t worry, the tumor is very small and with surgery and radiation, you will be fine.”
–1:55pm Wednesday, March 25, 2009: This was the moment Marge was told that the breast cancer had spread to her ribs. “But, don’t worry, the tumors are small, and with hormones, you will be fine.”
–4:43pm Monday, February 14, 2011: This was the moment Marge was told that the cancer had spread to the lining of her abdomen. “But, don’t worry the amount of cancer is very small, and with chemotherapy, you will be fine.”
–5:00pm Friday, December 6, 2013: This was the moment Marge was told that despite all the aggressive therapy she had received over the years, despite doing everything anyone had ever asked, the cancer was “terminal.”
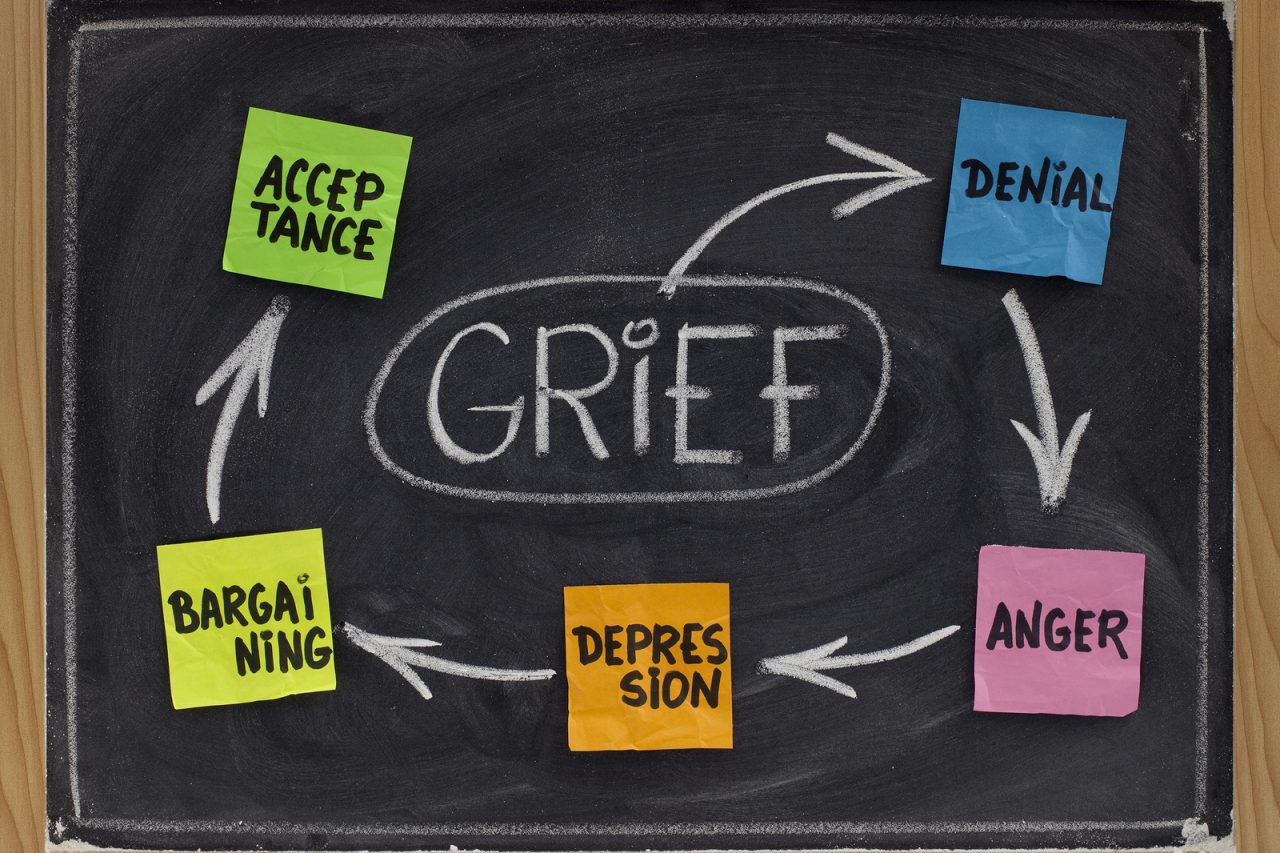
–11:15 pm Friday, December 6 2013: This was the moment when, late, in the dark, completely alone, Marge realized that for at least four years, ever since the cancer had come back in her bones, that the cancer had been only treatable and not curable and that the doctors, “had lied to me, and never told the truth,” and she vowed to sue them for every cent they owned.
I met Marge for a “second” opinion and confirmed that the cancer was growing rapidly in her abdomen and there was little that could be done. She was shocked. She was shocked to find out she was dying, and just as shocked to learn that her doctors had never explained that once breast cancer spreads it is almost always incurable and that every bit of treatment since the cancer had metastasized had been palliative.
Through her tears, Marge asked why her previous oncologist had not told her “the truth.” I explained that frequently doctors try to preserve “hope”, and tend to overstate the benefit of treatment and overestimate the likelihood and length of survival. Doctors may not have faith in each patient’s ability to cope with hard news and may believe that patients will “give up.”
Devastated to find her time was so short, likely weeks, Marge was even more upset she had failed to use the final years and months of her life “well.” Instead of retiring early and focusing on her grandchildren, instead of addressing precious items on her “bucket list,” instead of helping her family plan for a life without her, she had continued to work full-time and had devoted significant effort to activities that in retrospect seem frivolous. Like all cancer patients, she had been aware that life was precious, but Marge now focused her righteous and legal anger on the doctors who had failed to tell her that her life was almost gone.
The nature of the law means it is unlikely Marge can bring a successful lawsuit against her doctors for offering “false hope,” instead of cold reality. There are two elements to proving malpractice. The first the patient (“plaintiff”) must prove that the doctor (“defendant”) made an error and the second element is that the error lead to harm.
A doctor accused of being “too hopeful,” will probably explain that in his or her professional judgment, the patient could not emotionally handle more “truth” than was delivered and the doctor will claim that when he tried to be more direct, the patient denied reality and clearly only wanted to hear positive news.
Even if Marge could prove she asked for clear statistics and prognosis and that the doctor deliberately lied, it will be difficult to prove “harm.” Marge did not receive bad physical anticancer care, but she believes instead she received incomplete information. Her claim would be that she lost the opportunity to choose the life she might have wished, not that she lost the chance to live at all.
The doctor will claim that the patient lived happily, enjoying family, work and involvement in the community and therefore the treatment was successful. The doctor will state that in his or her experience given the “terminal” nature of the disease that it is very likely the patient would have become miserable and angry had more information been shared. In effect, the doctor will say that given a terrible situation, this was the best outcome.
The question for me is not whether a judge and jury would find against the doctor, rather the question resides more in the court of our hearts. Do not each of us have a right to decide our own futures? Should doctors act as our paternal guardians and decide, by the default of guarded communication, how we will live our lives? Are we so pathetically weak, like suckling babes, that we cannot guide our own lives?
Should not each doctor, at very least, say to each patient, “how much do you want to know,” and not assume we will melt in the harsh glare of bad news? Is telling difficult truths the sole responsibility of the doctor or is the burden on each of us to have the courage to ask?
Over the years, I have seen patients become obsessed with malpractice actions as they approach the end of their lives, consuming irreplaceable energy and time. While I was sympathetic with Marge’s anger, I encouraged her to move on. Each moment is precious and must be used well, and not on a vendetta which would not be resolved until long after she was gone, and likely not in her favor. Her focus must now be on her family, friends and on the quality of her life; but anger and loss will no doubt taint her memory.






24 Comments