Allow me to describe a recent case and ask your opinion. Today, you are the intake nurse at Happy Hospice and you are asked to evaluate Stan. This gentleman has incurable cancer, but treatment would probably prolong his survival. However, Stan has refused that treatment and been referred to you. It is your job to decide if he is “hospice appropriate.”
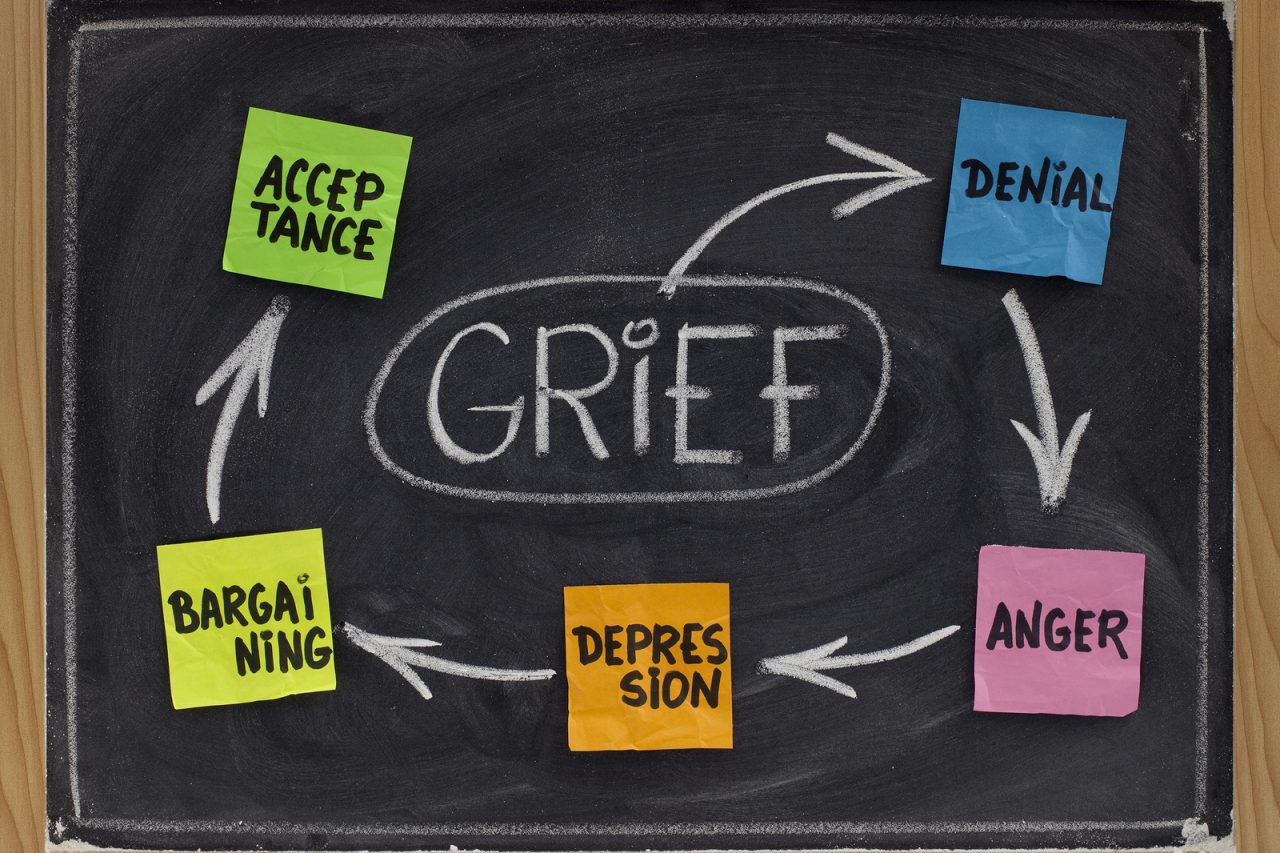
Why has Stan refused therapy? It is not that he denies there is cancer. Quite the opposite he can spout specifics of the disease. Stan is not bargaining for more life or fooling himself that hospice can somehow provide a fix. He is not depressed, at least in the sense of being suicidal. No, Stan would definitely love to live. Moreover, Stan does not accept that his time has come and therefore a good death is his only goal.
No, Stan feels one clear, emphatic emotion. Anger. Seething, pissed off, screaming to the sky, fury. He is enraged that his life has been cut short and all that is lost. He is livid about the intrusion of doctors, nurses, technicians, pain, nausea and every look of pity, sympathy, and self serving son-of-a-b****h “friend” who comes by his bed to give their phony, frightened, glad-it-is-you-not-me, good ridden wishes.
Stan sits before you. Jaw tight, eyes squinting, grimace fixed, hands clenched. His wife is on the other side of the room, exhausted from crying, her bloated gaze on the floor. The house has not been cleaned in weeks. Dishes spill from the sink, across the counter. The grass outside is long, a dusty car sits parked, one wheel on the lawn.
“Why do I want hospice? Because, I am sick of this s**t and if I am going to die anyway, at least you can make sure I do it at home and maybe without pain. But, if you can’t help me, well then I‘ll just do it myself.”
Not your typical hospice referral. No acceptance here. No peace. Not even the silent sorrow of loss. Just projected agony, which spits in the face of the disease, and in the face of life itself.
So, do you admit him as a hospice patient? How can you take a patient into your care when the whole reason that he refused treatment, is that he is too angry to cope? It is hard to make a case that he has carefully balanced his options. He is too upset to be open to details of therapy. The family communication is a mess. It seems doubtful that his decision to enter hospice represents informed consent. Is cancer the only reason to say “yes?”
Does Stan need to control his anger to really accept or be accepted into hospice? Does he need, “pre-hospice” counseling? Are you going to suggest he take a shot at chemotherapy?
As the referring doctor, I propose that Stan could be the ideal hospice candidate. Not the easiest, by far, but then we cut our teeth on the hard cases. Stan and his family have vast needs and the potential for help is great. This is the kind of patient that hospice may actually heal. Heal, not of the body, but the soul. If Stan is going to live out the rest of his life with any peace and if we are going to stop his anger from poisoning the generations of his family to follow, hospice may be the perfect therapy.
The basic tools of hospice are Stan’s best hope. Patience, listening, quality of life and a primary goal to serve the patient’s desires, mean that with time Stan may build trust. The emphasis on family and team, offers the chance that Stan will connect with members of the hospice service, and using that connection he can find comfort and help.
How far that healing will go, will depend on Stan, his family, his doctor and the skill of the hospice team. It will not be black and white, but settle somewhere in a range. At the failure side of the range, Stan throws you, the hospice nurse, out of the house this afternoon, goes in his room, never comes out, and dies a lonely, angry, destructive death.
At the radically successful end of possibility, is that Stan comes to find some calm and peace, generally accepts that the life that remains can be lived gently, talks to his wife, mends their personal pains and dies quietly at home. Perhaps, he even takes a break at some point to try active therapy, and returns to hospice when that choice has run its course. Of course, reality will be somewhere in between.
This is what palliative care and hospice are all about. We enter the end of life, much as we have lived the rest. Few of us are saints or angels. We snarl, bark, get confused, cry, and carry on. Our dysfunctions amplify and weakness lay bare. Nevertheless, with support, guidance and a kind ear, that which has brought us joy, satisfaction and love can come forth, and carry us through the darkest hour.






33 Comments