When counseling patients and families about end-of-life care, I try to focus on a simple, clear standard. Knowing that events are overwhelming and complex, I say, “Look at each treatment, each action and each moment and ask; How does it improve quality of life?” My goal is to reduce the choices during a chaotic time of life to the simple goal of comfort.
For example, most families are very concerned about nutrition and worry that the person they love may “starve to death.” I tell them that given the presence of a fatal disease, it is unlikely that eating will lengthen the patient’s survival and by stimulating the cancer, eating may even shorten life. Rather, the purpose of eating should be the quality of that moment. Families can rely on the simple standard, is the person hungry; do they want to eat? Something that tastes good may not change their body or the disease, but is the ultimate “comfort food.” Therefore, if the patient only eats a little or is not interested in food at all, that is OK, because then food is not a quality issue.
Another simple example is the long list of medications that burdens many of us, especially as we get older. For a patient receiving hospice or palliative care, that list should be reviewed by the same criteria; does it help quality of life? For most patients; pain medications, antidepressants or anxiety medicines would be “yes,” cholesterol and blood pressure medicines would be “no,” and blood thinners, “maybe.” So, what about chemotherapy?
I think it is crucial to understand the purpose of chemotherapy in each patient. We should endeavor to put chemo in the perspective of that person’s disease and goals. I suspect that one of the problems we have with end-of-life care, is the failure to explain to each patient what anticancer drugs can or cannot do. Studies show that a majority of patients receiving chemo for incurable disease believe that the treatment may still cure them.
Of course, in many diseases, chemotherapy may in fact result in cure. Stage IV Testicular Cancer is usually cured with chemo. Hodgkin’s Disease, acute leukemia, early stage breast and colon cancers, localized cervical cancer and many others are treated with medications, chemotherapy, with the goal being to get rid of the cancer forever or at least control it for many years. Usually these patients are willing to accept side effects, toxicity and a general decrease in quality of life, at least during chemotherapy, in order to be cured of the dread disease.
What about diseases which we often treat with chemo, but cannot be cured? Common examples are lung cancer, pancreatic cancer, advanced breast and colon cancers and metastatic prostate cancer. If these diseases are fatal, why do we treat them with drugs, at all? I propose that the failure to answer this question confuses patients and results in far more complications and suffering than is necessary or reasonable.
When giving chemotherapy, or any other anticancer therapy, when the cancer cannot be cured, the goal is palliative. By that, I mean the goal is to decrease pain, increase quality of life and perhaps help the patient to live a little longer. The goal is not cure. If chemo is just that, a comfort and quality tool, then each patient and family, when they are offered chemotherapy, should hear a version of my first words; “Look at this treatment, each dose of chemo and each visit to the office and ask; How does it improve the quality of life?”
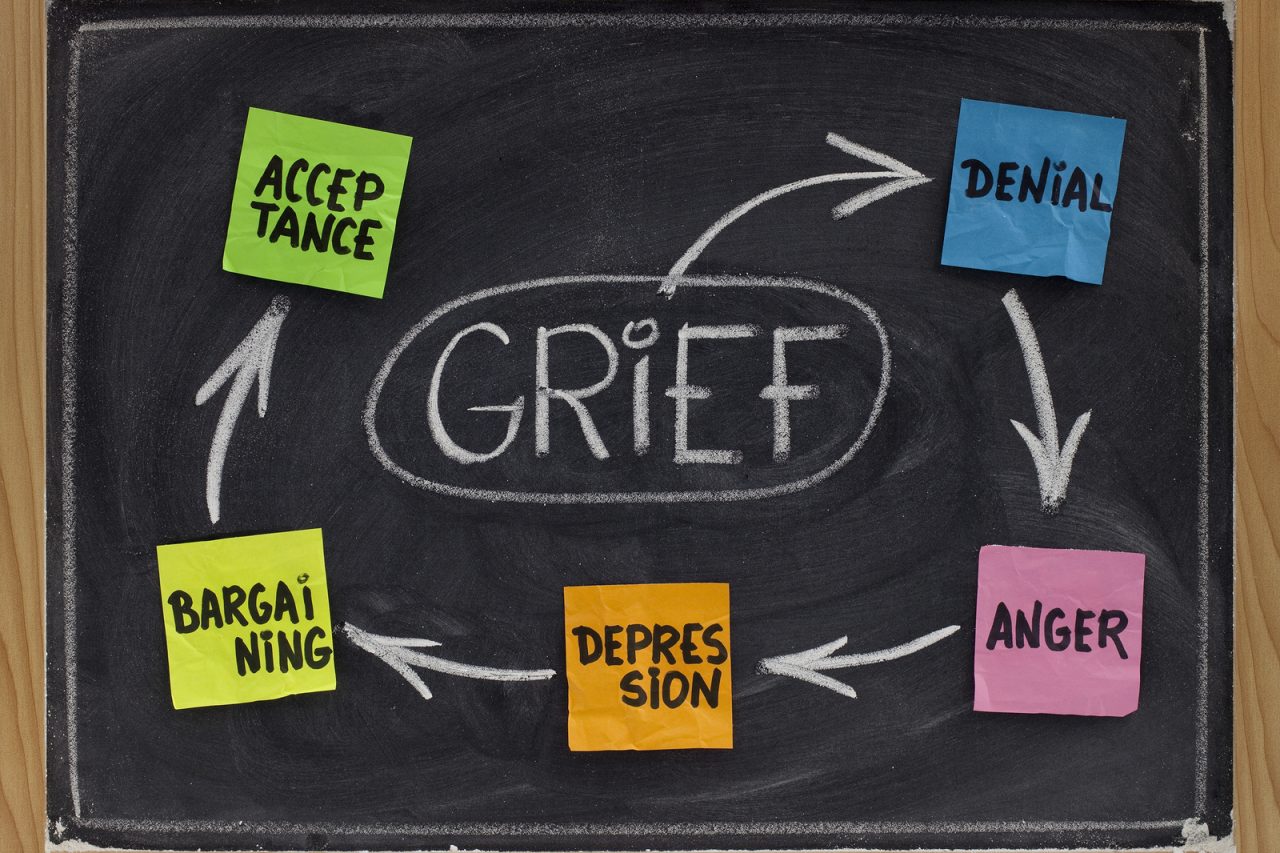
Having this conversation at the start, not just rushing into the first and second and even third course of chemo, week after month of toxic therapy, would help families set realistic goals and have reasonable expectations. Just like everything else, that the patient receives to treat the disease and its symptoms, families and patients should have the honest opportunity to balance personal goals with side effects and perhaps decide whether the time that therapy takes from day-to-day life is justified.
Doctors have a way of dominating medical care and taking control from patients and families. Only families can judge how the sacrifice of therapy affects the quality of each patient’s life. By viewing chemotherapy as a potential comfort measure, it would be easier to makes decisions during those final battles. Each person must hear, “we can help you decide, but it must be your choice. And one choice is to not do treatment at all.” Empowered by this knowledge each patient and family can better find quality during one of life’s most difficult journeys.





16 Comments