Her name is Joann; she has cancer. As that disease goes it is not much, probably curable, one of those “if you have to get cancer, this a good one.” Still, she sits across from me, her skin pale, eyes tight and she rhythmically grasps her cold, moist hands. She fails to gain any comfort from the knowledge that she is going to be OK. Why? I have not told her.
His name is Eric; he has cancer. As that disease goes it is bad, incurable, one of those “if you have to get cancer, do not choose this one.” He sits across from me, rocking slightly in the chair, making fleeting eye contact and tightly gripping both knees. He fails to gain any comfort from the knowledge that there is still a lot we can do and that we will control his pain and I will take care of him. Why? I have not told him.
Recently, a new patient sat down with me. She did not know my style or my belief in direct patient empowerment. She felt the need to educate me on how she wished to be treated. After I finished taking her history and doing a careful exam, but before I began teaching her about diagnosis, therapy and prognosis, she looked me in the eye and said. “Doctor, whatever you do, you have to tell me everything. You have to be honest with me. I need to know, so I will not be scared.”
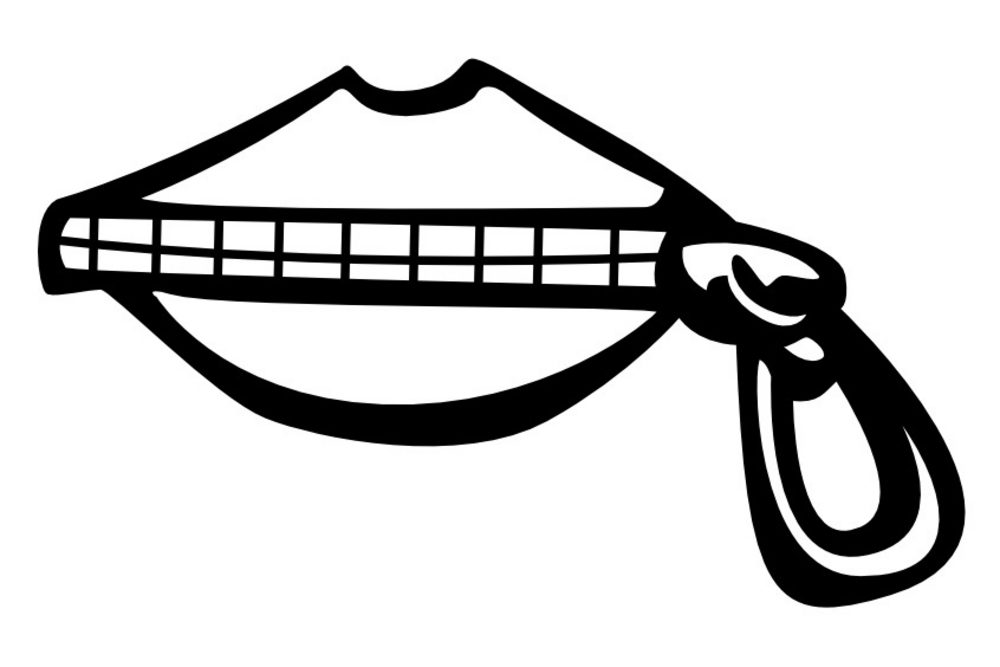
Doctors spend a lot of time lying to people. Perhaps, that is the wrong word. Doctors spend a lot of time holding back the truth and doling out bad news in small pieces. We may plan to eventually tell the complete story, but time passes, new events interfere and our patients never gain a full grasp of what is happening. We do this out of love and compassion, not wishing to cause pain or overwhelming anxiety. Nonetheless, by leaving much unsaid and in the dark, we cause fear and amplify suffering.
There are two basic facts we need to understand and incorporate into medical practice. The first is that most people are extremely strong and capable of coping with the worst medical news. It is not that anyone will be thrilled to learn about a dire prognosis, but with support and time, we can handle it. Doctors and families often underestimate the inner strength of patients. We are so concerned that someone we care for will give up, we give up on them.
The second is that people need to know the truth so that they can concur fear and plan their lives. When the unknown is rapped in sterile halls, sharp needles, stern physicians and stamped with the word “cancer,” terror has no stronger name. Given a complete picture of what is happening, patients and families can organize their emotions and plan lives to cope with what is to come. In the absence of an understanding of reality all they have is thin hope, and that makes for a flimsy blanket.
Now, to be clear, the communication I am prescribing is not:
“You have cancer. You are screwed. Get your affairs in order.”
I am talking about systematic, compassionate, supportive education:
This is what we have found. Do you understand? This is the diagnosis. Do you understand? This is the likely prognosis. Do you understand? These are the treatment alternatives. Do you have any questions? In addition, where reasonable, it is vital to include the extremely rare statement; “you do not have to do anything, it is up to you.”
A back and forth patient conversation, which depending on the patient’s comprehension and need, may occur over several meetings. The patient needs to be informed and kept in the loop regarding changes, both good and bad. The doctor is the learned advisor; the patient is in charge.
The truth shall set you free. This is freedom from the unknown, freedom from pain and freedom to live your life as you wish. Doctors, caregivers and families must empower each patient with the knowledge to guide their own futures. With compassion, they can walk through the blackest night. It our job to light the darkness.




15 Comments