Not long from now, the last cancer will be defeated, and even today most with the dread disease survive. However, many still fall. This leaves us with one of the toughest questions of life. How long do you continue to fight, when death is certain? When does striving become vain hope which drains quality and creates only suffering? What makes struggle worth the pain; when is it time to yield?
This is a highly personal decision, which each of us can decide only for ourselves. I have met young people who when faced with incurable disease, immediately decide that life was over, and accepting only comfort, make no attempt to delay death. I have known frail very senior patients, who faced with an incurable disease, demand every treatment, the end of their lives announced by the compressions of CPR. Is either path right or wrong? I do not know. Nevertheless, the certainty of these decisions demands that we consider this future, as best we can, before these events occur.
In talking to patients with chronic fatal disease, one image, which seems to help, is that of climbing mountains. If you have cancer, you face a series of medical and emotional events. The first will be the symptoms that announce the disease, such as pain, swelling or bleeding. The next event will be undergoing tests to get a diagnosis. Then, the first treatment. Each of these is a hill or mountain over which you will need to hike and each follows the other.
As you get over one rise, and recover from that climb, in front of you stands the next hill. Often the ascent in front is higher and harder than the one just completed. You must climb it, even though the mountain behind has depleted you. Sometimes there will be a wide valley or plain between the mountains, where you can rest and heal. During other parts of the journey, the foothills of one mountain will stumble immediately into the next rising slope. At times, you will reach the top, just to realize it was a mirage and the real summit is higher still.
When cancer relapses or spreads, the treatment may demand more sacrifice. The side effects are more severe, precious energy lost, time away from family increases, and the opportunity to simply live is taken away. More mountains rise in front of you.
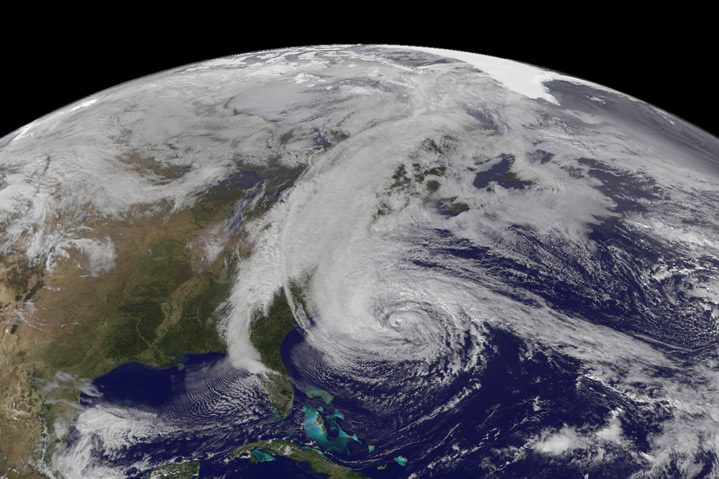
Having a fatal disease means that with time the mountains will get closer and higher, the climbs more savage, and the toll on your life and body will get worse. We may fool ourselves that even though the disease has relapsed that if we scale the next Himalayan crag, we will finally get to rest. But, since death defines human life, at some point there will come a mountain which is so steep and so hard and causes us so much suffering, that we will die on its rocky side or plummet into a ravine.
I would not pretend to know when for each disease, each person, each life, the time has come to take off the hiking boots, and sit by the fire. The range of rising mountains reminds me that the path we tread, at the end of our lives, is a balance between hope’s struggle, and the comfort which some may find in acceptance. The analogy can test how we measure choices in treatment and in daily life. For each of us what is important and gives meaning to our lives, is balanced with what we sacrifice.
The question is whether we will have the wisdom to recognize that the time has come not to climb, but to rest in the warm valley. The peak of Everest is a crystal pure image of awe, power and beauty, but for most, it is a place of fantasy, where there is no air and the wind is as cold as death.




16 Comments