Let me be clear. I have spent a career, my adult life, 80 hours a week, 131,000 hours, fighting the dread disease; every method, every drug, every machine, every medical technique, every sinew of my being, to control or cure malignancy. A synopsis of my existence will say, “fought cancer.” Nonetheless, let us take a step back, if just for a moment, and reflect on the idea of saying, “no.”
In 2015, approximately 60% of patients with cancer will be cured. This is a remarkable improvement over a generation ago, when the disease was usually fatal. Sadly, this means that four out of ten cancer patients still die of their disease. This is a terrible, tragic truth. It is also a silent truth.
Nearly 100% of patients with metastatic lung cancer will die. However, studies indicate that 70% of patients with advanced lung cancer believe that the purpose of chemotherapy is to cure. Similar data and experience exists for most other aggressive cancers. Patients often lack a realistic understanding of what treatment can and cannot do.
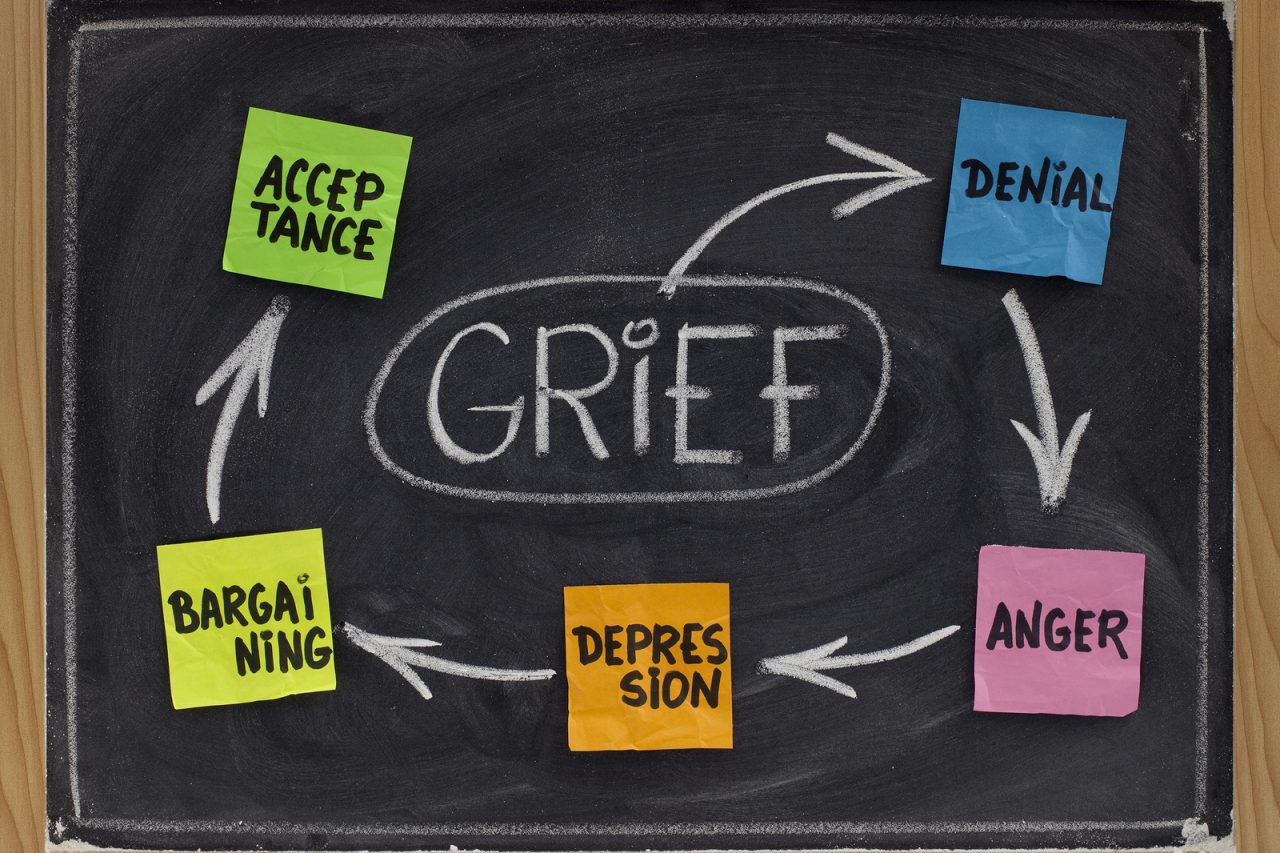
Is this denial? Are patients unwilling to face the harshest reality? Sometimes. There is a limit to what each of us can handle; how much anxiety, threat and bad news we can cope with at any moment.
However, I believe that one reason many patients do not have a realistic understanding of the limits of medical therapy is that the list of treatment choices presented by their treating doctors includes drugs, surgeries and radiation, but rarely does it include the words, “and if you decide, you do not have to do anything to treat the cancer at all.”
There is no law that if a treatment exists with a small chance of extending survival for a small amount of time, that it is necessary to take that treatment. Just as there is so much bad news each of us can handle, so there may be too much traumatic therapy with which we can cope. There is a hard line for each of us after which life is not worth living.
Still, if any sort of treatment is available, no matter how limited the benefit, doctors rarely offer “quality and comfort,” instead of active therapy. We do not put into perspective the reality of a fatal disease, the potential complications of medical treatment, or give a clear picture of what may be coming in the weeks and months ahead.
We act as if not providing therapy is “giving up,” instead of reassuring each patient that we will never give up on them or on life, but that treatment may cause more suffering than benefit. We do not allow each patient the opportunity to balance their hopes, dreams and fears with the reality of what can actually be achieved.
Let me be clear. Even though I have spent my life fighting cancer, I do not have the ability to judge what life means to you. Each of us should have the freedom, opportunity and duty to decide, for ourselves, how to live life, especially at its end. I hope I can step back so that each of my patients has the chance to reflect and consider their future, and even if they to say “no,” still be by their side.






18 Comments